Introduction: As gene therapy for sickle cell disease (SCD) continues to advance, there is growing potential for genomic screening to be utilized in determining eligibility for this therapy. With this comes the ethical obligation to look for secondary findings (SF) in clinical exome and whole genome sequencing. The American College of Medical Genetics (ACMG) has issued recommendations for returning SF in clinical care and annually updates a list of pathogenic variants. This abstract reports on our experience with returning SF to a SCD study population in research.
Methods: The INSIGHTS Study (NCT02156102) is a cross-sectional perspective research study examining phenotypic variation in adults living with SCD. All study participants consented to whole genome sequencing (WGS) and agreed to have secondary genomic findings returned. Participants completed the study between 2014-2020. To date, 264 samples have undergone WGS, performed at the National Institutes of Health Intramural Sequencing Center.
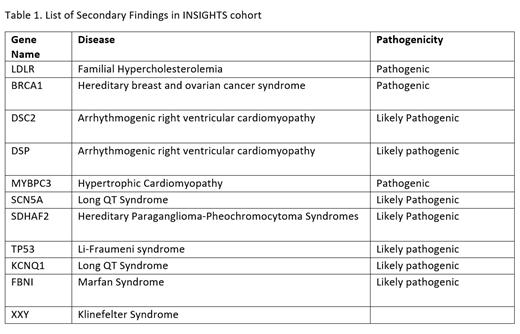
Results: In accordance with the guidelines issued by ACMG, 12 participants (4.5%) were found to have genetic variants on the current list (ACMG SF v3.2) that were eligible for return (Table 1). Additionally, one participant was found to have a sex chromosome aneuploidy, and after a full ethics board review, it was determined this result should also be returned based on its clinical actionability and the risk/benefit analysis. Of these 12 participants, three were deceased. One participant was already aware of the secondary finding. We contacted the remaining eight participants and as of July 2023 five participants provided a new sample for CLIA confirmation. Results were returned in consultation with the Secondary Findings Consult Service at the National Human Genome Research Institute, which provided a genetic counselor. Participants met with a clinical member of the study team and the genetic counselor either by telephone or in person. The consultation consisted of sharing the result and associated risk of disease, obtaining pertinent medical history and detailed family history, and providing recommendations and referrals.
Discussion: With the expansion of genomics into hematological and sickle cell disease research, it is paramount that the implications of its integration continue to be examined. The responsibility of the research team to facilitate and/or provide ancillary care to their study participants to best support them in receiving SF results should be clearly defined. In addition, each patient will have unique needs that should be considered and may require specialized assistance. Questions on how the SF affects the patient's primary diagnosis will need to be addressed, which will require a multidisciplinary approach to care. These consultations will require a high level of patient coordination and clinical support. It is important that these patient encounters 1) involve a known and trusted medical professional; 2) provide accurate and understandable information on the genomic finding, usually by a genetic counselor; and 3) refer the patient to an appropriate clinical provider who is an expert in that disease.
Disclosures
No relevant conflicts of interest to declare.